Losing a tooth can affect not only your smile but also your overall oral health and confidence. If you’re wondering when should you consider dental implants, this guide will walk you through everything you need to know about this popular and effective tooth replacement option.
Dental implants have revolutionized restorative dentistry by providing a durable, natural-looking solution that can last a lifetime with proper care. But how do you know if they’re right for you? Let’s dive in.
What Are Dental Implants?
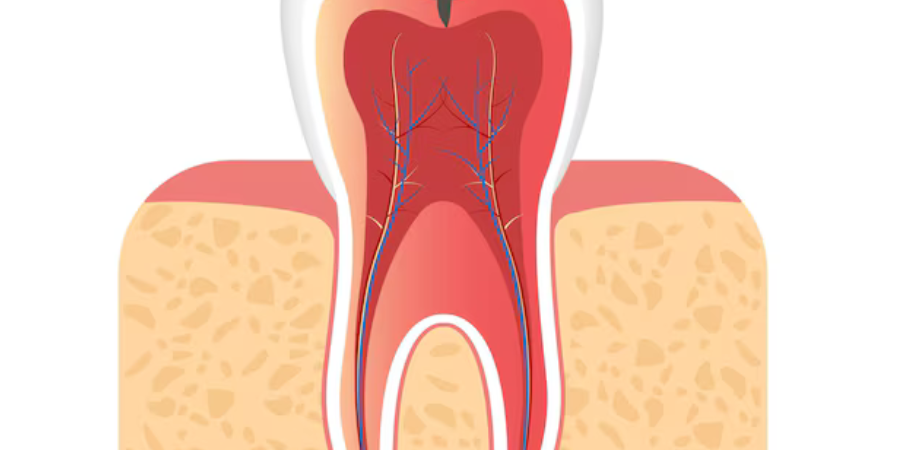
Dental implants are artificial tooth roots made of biocompatible titanium, surgically placed into the jawbone. Once integrated, they serve as a sturdy foundation for crowns, bridges, or dentures.
Why Choose Implants Dental?
Compared to traditional dentures or bridges, dental implants offer superior stability, functionality, and aesthetics. They help preserve jawbone density and prevent bone loss, maintaining your facial structure.
When Should You Consider Dental Implants?
- You Have One or More Missing Teeth
If you’re missing teeth due to injury, decay, or extraction, dental implants can replace them individually or support multi-tooth restorations.
- You’re Tired of Dentures That Don’t Fit Well
Traditional dentures can slip or cause discomfort. Implants dental secure dentures firmly in place, improving chewing efficiency and confidence.
- You Want a Long-Term, Durable Solution
Dental implants are designed to last decades, often a lifetime, unlike bridges or dentures which may need replacement every 5-10 years.
- You Have Healthy Jawbone and Gums
Good bone density and healthy gums are essential for implants to integrate well. If you’ve experienced bone loss, bone grafting may be an option before implants.
- You’re Committed to Good Oral Hygiene
Successful dental implants require diligent oral care and regular dental visits.
Comparing Dental Implants with Other Tooth Replacement Options
| Option | Longevity | Appearance | Comfort | Bone Health | Maintenance |
| Dental Implants | 15+ years (often lifetime) | Natural-looking | Very comfortable | Preserves bone | Similar to natural teeth |
| Bridges | 5-15 years | Good | Moderate | Does not preserve bone | Requires cleaning around bridge |
| Dentures | 5-10 years | Varies | May slip | Can accelerate bone loss | Needs daily cleaning and adhesives |
Benefits of Dental Implants
- Improved Chewing and Speaking: Implants function like natural teeth.
- Enhanced Confidence: Look and feel great with a permanent solution.
- Preservation of Facial Structure: Prevents jawbone deterioration.
- No Impact on Adjacent Teeth: Unlike bridges, implants don’t require grinding neighboring teeth.
- Easy Maintenance: Brush and floss as usual.
Expert Tips Before Getting Dental Implants
- Schedule a thorough dental evaluation, including X-rays or 3D scans.
- Discuss your medical history, including any conditions like diabetes or smoking habits that can affect healing.
- Ask about the implant process timeline — it can take several months including healing.
- Maintain excellent oral hygiene before and after the procedure.
- Follow your dentist’s post-surgery care instructions strictly.
What to Expect During the Dental Implant Process
- Consultation and Planning: Customized treatment plan.
- Implant Placement Surgery: Titanium post inserted into the jawbone.
- Healing and Osseointegration: The implant fuses with bone (3-6 months).
- Abutment Placement: Connector piece attached.
- Crown or Prosthetic Attachment: Final tooth or denture secured.
When Not to Choose Dental Implants
Dental implants might not be suitable if you have:
- Severe bone loss without options for grafting
- Uncontrolled chronic illnesses
- Smoking habits that interfere with healing
- Poor oral hygiene habits or unwillingness for regular dental visits
Share Your Thoughts!
Have you considered implants dental or already have dental implants? What was your experience like? Share your story, ask questions, or leave tips in the comments below. Don’t forget to share this post if you found it helpful!
Conclusion: Is It Time to Consider Dental Implants?
Deciding when you should consider dental implants depends on your oral health needs, lifestyle, and personal preferences. For many, implants dental offer a reliable, natural-feeling solution to missing teeth that can enhance quality of life for years to come. Consult with your dentist today to explore if implants are the right choice for you!