Dental crowns, commonly known as caps, play a significant role in restorative and cosmetic dentistry. They cover a damaged, decayed, or weakened tooth, restoring its shape, strength, and appearance. For many, dental crowns are essential in maintaining a natural smile, improving oral health, and preventing further dental issues. If you’re considering a dental crown or simply want to understand when and why you might need one, this guide will clarify everything you need to know.
What Are Dental Crowns?
A dental crown is a custom-made cover placed over a tooth to protect and restore its function. These crowns are crafted to look, feel, and function like natural teeth, blending seamlessly into your smile. Crowns can be made from various materials, including porcelain, ceramic, metal alloys, resin, or a combination. The choice of material often depends on the location of the crown, your specific dental needs, and your dentist’s recommendation.
When Might You Need a Dental Crown?
There are several scenarios in which a dental crowns can be beneficial, both for functional and cosmetic reasons. Some of the most common reasons include:
- To Protect a Weak Tooth: A tooth that’s been weakened by decay or injury may need reinforcement to prevent it from breaking or suffering further damage. In these cases, a dental crown acts as a shield, offering support and stability to the weakened tooth structure.
- To Restore a Broken or Severely Worn Tooth: Teeth can crack, chip, or wear down due to accidents, grinding, or age. A crown can restore the structure and strength of a damaged tooth, enabling you to chew and speak comfortably without pain or discomfort.
- After a Root Canal Treatment: A root canal procedure removes infected tissue from inside the tooth, often leaving it fragile and prone to cracking. Placing a crown on top of a root canal-treated tooth provides protection, sealing it from bacteria and preserving its function.
- To Support a Dental Bridge: If you’re missing one or more teeth, a dental bridge may be used to fill the gap. Crowns are typically placed on the teeth adjacent to the gap, serving as anchors for the bridge to restore a full and functional smile.
- For Cosmetic Reasons: Crowns are also a popular choice for cosmetic purposes. If a tooth is discolored, misshapen, or has minor alignment issues, a crown can improve its appearance, helping you achieve a more confident smile.
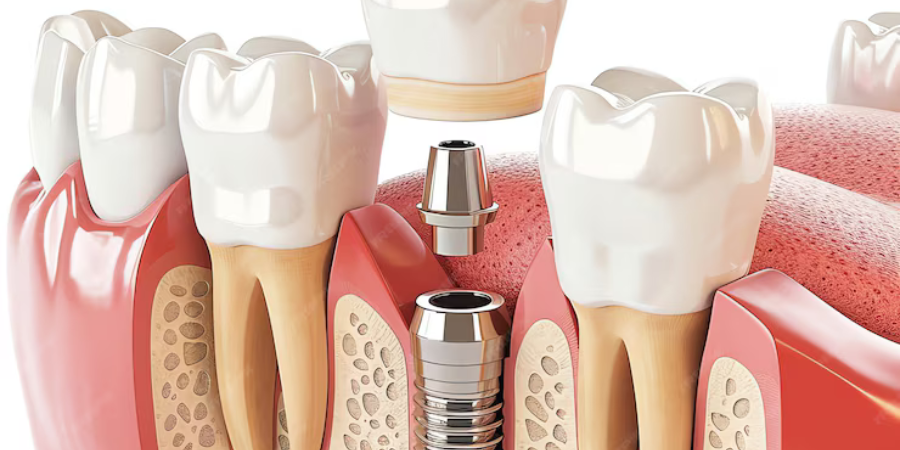
- To Cover a Dental Implant: When a dental implant is placed to replace a missing tooth, a crown is attached to the implant to complete the restoration. This crown functions just like a natural tooth, restoring appearance and functionality.
The Dental Crown Procedure: What to Expect
The process of getting a dental crown typically involves two visits to the dentist:
- Initial Consultation and Tooth Preparation: During the first visit, the dentist will examine your tooth, take X-rays, and prepare it for the crown. This may involve reshaping the tooth by filing down the damaged areas to make room for the crown. If there’s extensive decay or damage, the dentist might first place a filling to build up the tooth structure. Once the tooth is prepared, your dentist will take impressions to create a model for the custom crown. This ensures a precise fit, so the crown feels comfortable and functions well.
- Crown Placement: When the custom crown is ready, you’ll return to have it fitted and cemented onto your tooth. Your dentist will check the crown’s fit and color to ensure it matches your natural teeth, then bond it securely in place.
In some cases, same-day crowns may be available. Using advanced technology, some dentists can create and place crowns within a single appointment, eliminating the need for a temporary crown and reducing wait time.
Types of Dental Crowns: Which Material is Right for You?
The type of material for your crown depends on factors like the location of the tooth, aesthetics, and budget:
- Porcelain or Ceramic Crowns: These are popular for their natural look and are often used on front teeth. They blend well with natural teeth, making them ideal for people who prioritize aesthetics.
- Metal Crowns: Made from alloys like gold or platinum, metal crowns are highly durable and resist wear and tear, making them suitable for molars. However, they’re noticeable, so they’re not usually chosen for visible teeth.
- Porcelain-Fused-to-Metal (PFM) Crowns: These combine the strength of metal with the aesthetic appeal of porcelain. They’re durable and can be used for both front and back teeth, though the metal underneath may sometimes show as a dark line along the gum.
- Resin Crowns: While they’re more affordable, resin crowns are generally less durable and may wear down over time. They’re often used as a temporary solution.
- Zirconia Crowns: Zirconia is a strong, biocompatible material that combines the aesthetics of porcelain with the durability of metal. Zirconia crowns are popular for their longevity and natural appearance.
Caring for Your Dental Crown
While a dental crown is designed to be durable, it still requires care to maintain its longevity:
- Practice Good Oral Hygiene: Brush and floss daily, paying special attention to the gum line where the crown meets your natural tooth. This area can be prone to plaque buildup, which could affect the crown.
- Avoid Hard Foods: Biting down on hard objects like ice, popcorn kernels, or pens can damage your crown. Try to avoid these as much as possible to prevent chipping.
- Schedule Regular Dental Checkups: Visiting your dentist regularly allows them to monitor the health of your crown and the surrounding teeth, addressing any issues before they escalate.
- Use a Mouthguard if Needed: If you grind your teeth at night, ask your dentist about a mouthguard to protect your crown and natural teeth from wear.
Benefits of Getting a Dental Crown
Opting for a dental crown offers several advantages:
- Preserves Natural Teeth: A crown protects a compromised tooth, preventing the need for extraction.
- Enhances Aesthetics: Crowns can restore the appearance of damaged or discolored teeth, enhancing your smile and boosting self-confidence.
- Improves Functionality: With a dental crown, you can chew, speak, and smile comfortably, knowing that your tooth is fully supported and functional.
- Durability: With proper care, crowns can last between 10 to 15 years or longer, making them a long-term investment in your oral health.
Is a Dental Crown Right for You?
If you’re experiencing tooth pain, have a broken or damaged tooth, or are dealing with cosmetic concerns, a dental crown might be the solution. Consult with your dentist to determine if a crown is the best option for your needs. They can help you choose the right type and material based on your preferences and budget, ensuring that you receive a crown that enhances both function and aesthetics.